ANTI-MICROBIAL RESISTANCE (AMR)

CONTEXT :
- Anti Microbial Resistance is a very high priority on the health agenda of the G20 countries.
MORE ABOUT THE NEWS :
- Anti-microbial resistance (AMR) is an urgent global public health threat that is driven at large by injudicious anti-microbial use across human, animal, and plant health sectors.
- Often referred to as a silent pandemic, it is one of the top 10 global health threats facing humanity according to WHO.
- It was in 2015, that World Health Assembly (WHA) adopted the Global Action Plan on AMR.
- As of now, 170 countries have established multi-sectoral National Action Plans (NAPs).
- WHO has declared that AMR is one of the top 10 global public health threats facing humanity.
WHAT IS ANTI-MICROBIAL RESISTANCE (AMR)?
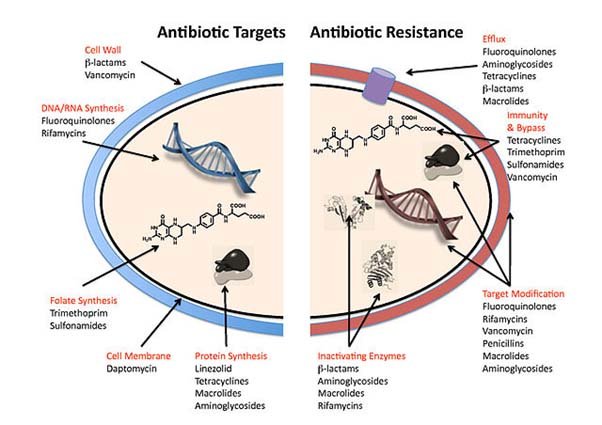
- Antimicrobial resistance (AMR) is the ability of microorganisms to persist or grow in the presence of drugs designed to inhibit or kill them.
- Antimicrobial Resistance (AMR) occurs when bacteria, viruses, fungi and parasites change over time and no longer respond to medicines making infections harder to treat and increasing the risk of disease spread, severe illness and death.
- As a result of drug resistance, antibiotics and other antimicrobial medicines become ineffective and infections become increasingly difficult or impossible to treat.
WHY IS IT A GLOBAL CONCERN?
- AMR is not a new post-pandemic threat but has been on the rise for many years.
- Research suggests that almost every major public health emergency since the past century has resulted from the crossover of pathogens from animals to humans.

- An estimated 4.95 million deaths were associated with bacterial AMR and 1.27 million deaths were directly attributed to bacterial AMR.
- It also showed that AMR is a leading cause of death around the world with a magnitude at least as large as major diseases such as HIV and malaria, enveloping its highest burden in low-resource settings.
- Antibiotics are becoming increasingly ineffective as drug-resistance spreads globally leading to more difficult to treat infections and death.
- The cost of AMR to national economies and their health systems is significant as it affects productivity of patients or their caretakers through prolonged hospital stays and the need for more expensive and intensive care.
CAUSES OF AMR

- Antimicrobial resistance is mainly caused by the overuse of antimicrobials.
- This leads to microbes either evolving a defense against drugs used to treat them, or certain strains of microbes that have a natural resistance to antimicrobials becoming much more prevalent than the ones that are easily defeated with medication
- Although many microbes develop resistance to antibiotics over time though natural mutation, overprescribing and inappropriate prescription of antibiotics have accelerated the problem.
- It is possible that as many as 1 in 3 prescriptions written for antibiotics are unnecessary.
- The use of antimicrobials in animal and plant production is influenced by an interplay of many factors:
- Burden of diseases that are otherwise preventable through modification of environmental hygiene, nutrition, husbandry and other management practices.
- Limited access to animal and plant health experts, as well as limitations in training and support for these experts.
- The use of antimicrobials as growth and production promoters in animals.
- Lack of regulation and oversight of the use of antimicrobial drugs.
- Over the counter or internet sales that make antimicrobial drugs readily available.
- Availability and use of substandard and falsified antimicrobials.
- Lack of awareness regarding good practices, leading to excessive or inappropriate use.
- Anthropological, sociocultural, political and economic factors that pose barriers good practices.
GLOBAL INITIATIVES TO TACKLE THIS ISSUE
- Global Action Plan on Antimicrobial Resistance (GAP): Globally, countries committed to the framework set out in theGlobal Action Plan1 (GAP) 2015 on AMR during the 2015 World Health Assembly and committed to the development and implementation of multisectoral national action plans.
- Tripartite Joint Secretariat on Antimicrobial Resistance: Tripartite joint secretariat (FAO, OIE and WHO) has been established and is hosted by WHO to drive multi-stakeholder engagement in AMR.
- Interagency Coordination Group (IACG) on AMR: It was convened by the Secretary-General of the United Nations after the UN High-Level Meeting on Antimicrobial Resistance in 2016.
- World Antimicrobial Awareness Week (WAAW):WAAW was previously called the World Antibiotic Awareness Week. From 2020, it will be called the World Antimicrobial Awareness Week.
- It is a global campaign that aims to raise awareness of antimicrobial resistance worldwide.
- Global Antimicrobial Resistance and Use Surveillance System (GLASS):WHO launched it in 2015 to continue filling knowledge gaps and to inform strategies at all levels.
- GLASS has been conceived to progressively incorporate data from surveillance of AMR in humans, surveillance of the use of antimicrobial medicines, AMR in the food chain and the environment.
- Global Antibiotic Research and Development Partnership (GARDP): A joint initiative of WHO and the Drugs for Neglected Diseases Initiative (DNDi), GARDP encourages research and development through public-private partnerships.
STEPS TAKEN BY THE GOVERNMENT OF INDIA
- To prevent the Over the counter sales of antibiotics, the central drug standard control organization (CDSO) prohibits medical stores from selling 24 key antibiotics without a doctor’s prescription.
- India’s Red Line campaign: Which demands that prescription-only antibiotics be marked with a red line, to discourage the over-the-counter sale of antibiotics– is a step forward.

- National Health Policy, 2017, terms antimicrobial resistance as one of the key healthcare issues and prioritizes the development of guidelines regarding antibiotic use and check on restricting the growth of antibiotics.
- The National Action Plan on Antimicrobial Resistance (NAP-AMR) 2017 has assigned coordinated tasks to multiple government agencies involving health, education, environment, and livestock to change prescription practices and consumer behaviour and to scale up infection control and antimicrobial surveillance.
- FSSAI has set certain guidelines limiting the antibiotics in food products such as fish and honey.
NEED FOR COORDINATED ACTION :
- The need to develop policies, invest in research and build the ecosystem to strengthen the connection between environment, human, and animal health.
- India has always accorded top priority to One Health and AMR and was one of the first few countries which developed a comprehensive National Action Plan (2017-21).
- Building on the principle of “Atmanirbharta” or self-reliance and acting upon the traditional ethos of “Vasudhaiva Kutumbhkam” or the world as one family, the country has worked relentlessly to offer health solutions as a service to humanity.
- Covid-19 was an example where India led the war against the pandemic from the front, playing an exceptional role in developing high-quality and cost-effective healthcare interventions from indigenously developed vaccines not just for itself, but over 100 countries, to offering Co-WIN platform as a digital public good to the world, to being self-reliant in diagnostics, masks, and PPEs.
- With India now taking over the presidency of G20, it is imperative that we take this agenda forward considering that AMR is one the topmost health priorities.
- The Global Call to Action on AMR has also urged the G7 and G20 countries for a continued and renewed commitment to implement their NAPs and thus, through a coordinated approach, ensure the flow of investment into the national and multi-sectoral action plans.
WAY FORWARD
- Some of the immediate steps to tackle global AMR concerns include launching a Global One Health Consortium having a common vision and mission, connecting health targets and policies with SDGs.
- Ensuring One Health is center staged, prioritising research for new diagnostics, antibiotics, vaccines, and building a strong demand driven market to ensure an assured supply and well-structured supply chain.
- Sufficient scientific data needs to be generated to help drive evidence-based policy decisions.
- BAlso as human health issues are getting discussed, it is time to focus our attention on animal and environmental health monitoring.
SOURCE : THE HANS
SYLLABUS : MAINS, GS-3 HEALTH